What is ASD (Atrial septal defect)?
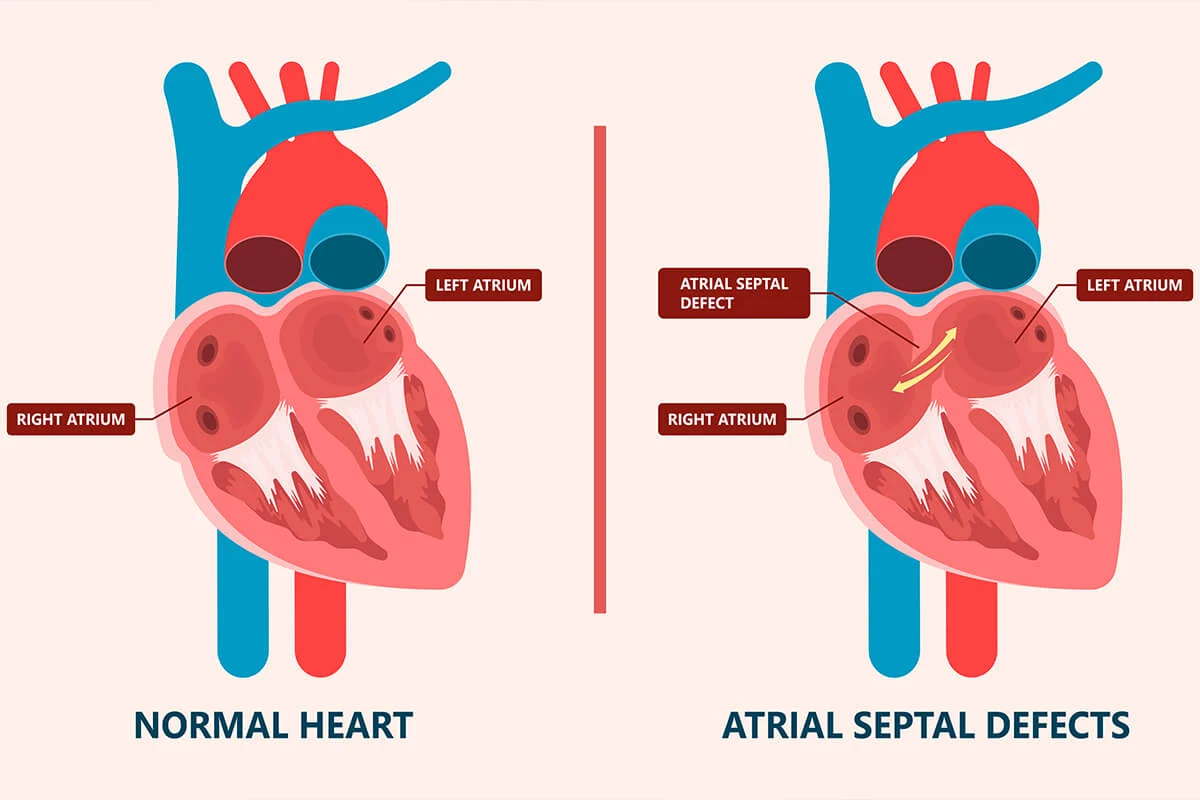
The presence of a congenital hole in the septum, which separates the right and left atria (auricles) of the heart, is known as an atrial septal defect (ASD).
Table of Contents
In the presence of ASD, a portion of the clean blood in the left atrium passes to the right atrium, leading to an increase in the volume of blood that the right heart needs to pump to the lungs.
Over the years, the high volume of blood flowing to the right heart and pumped to the lungs causes the right atrium (auricle) and the right ventricle (ventricle) to enlarge.
This can lead to an increase in blood pressure in the pulmonary artery (pulmonary hypertension) and ultimately right heart failure. Right heart failure and pulmonary hypertension can reduce the patient’s quality of life and can lead to death.
Additionally, when right heart failure and pulmonary hypertension develop, blood clots that form in the leg veins can pass through this hole (ASD) and travel to the brain, causing blockages in the brain vessels and resulting in strokes.
Why is ASD closed?
Small ASDs (holes) allow a minimal amount of left-to-right blood flow, so they do not affect the patient’s life and do not cause problems even in advanced age.
Therefore, there is no need to close small ASDs (holes). On the contrary, attempting to close small ASDs (holes) through surgery or a minimally invasive procedure would unnecessarily expose the patient to the risks associated with closure.
When the ASD is large, and the volume of blood passing from the left to the right through the ASD is dangerously high and damaging to the heart, closure is necessary and beneficial for the patient. If a significantly large ASD is left untreated, it can cause irreparable damage to the heart cavities and pulmonary arteries.
How to turn off ASD?
Surgical closure: When an ASD is not suitable for non-surgical closure methods, it needs to be closed through surgery. During the surgery, the surgeon opens the right atrium, locates the hole, and closes it by stitching or patching it.
The procedure inside the heart is the same for all surgical techniques, but the method of opening the chest differs among surgical approaches. In the initially developed and most commonly performed surgical technique, the chest is opened from the midline, extending from the neck to the abdomen, and the ASD is repaired.
This open-heart surgery leaves a significant scar on the patient’s chest, which especially young individuals may find undesirable. A more aesthetically acceptable surgical method involves making an approximately 20 cm incision extending from underneath the right breast to the side of the breast, opening the chest cavity.
This approach results in the majority of the surgical scar being concealed beneath the breast in women, making it more visually acceptable. In the more aesthetically refined approach developed in recent years, a 6-8 cm incision is made on the side of the right breast.
A camera is inserted through this incision into the chest cavity, allowing the surgeon to perform the operation while viewing the screen. Following the surgery, an incision of approximately 6-8 cm remains on the side of the right breast.
In this minimally invasive surgical approach, the patient can stand up, be discharged from the hospital, and return to normal life earlier. The extent and appearance of the surgical scar should be discussed with the surgeon beforehand.
Non-surgical closure of ASD: Most ASDs are suitable for non-surgical closure, and in recent years, a small number of patients undergo surgery due to ASD. In appropriate cases, non-surgical closure should be preferred over surgery.
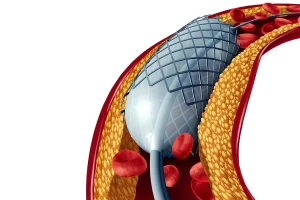
In the non-surgical ASD closure method, a needle is inserted through the femoral vein in the groin, and a guide wire is sent from there to the heart, passing through the ASD (hole). A vascular sheath with a thickness of 3-5 mm is similarly inserted from the groin and advanced to the heart, passing through the ASD and leaving the tip in the left atrium.
ASD closure devices are two disc-shaped devices connected in the middle. The selected closure device suitable for the ASD is advanced through the vascular sheath from the groin, passing through the hole. One disc of the closure device is opened in the left atrium, and after being pulled back a bit, it is placed on the ASD with the tip positioned in the left atrium.
Then, the second disc of the closure device is opened in the right atrium, and the device is positioned to cover the hole from both sides. Before the device is released, it is ensured that the ASD is properly closed and that the implanted device does not harm other parts of the heart.
If everything is appropriate, the procedure is terminated, and the closure device is left on the ASD. The endocardium, the cell layer lining the inside of the heart, covers the closure device, and within an average of 3-6 months, the closure device is completely covered with endocardial cells.
The closure device remains there permanently. Some individuals may be allergic to the materials used for these closure devices and should be questioned before the procedure. The non-surgical ASD closure procedure takes about 1 hour on average, and the patient may need to be sedated for about half an hour during the procedure.
This is not general anesthesia but is described as deep sedation or deep sleep, and the patient is awakened immediately after the procedure. In some cases, the procedure can be performed while the patient is awake.
After the procedure, the patient remains in bed for at least 6 hours and stays in the hospital overnight, being discharged in the morning.
To prevent clot formation on the closure device, it is recommended to use clopidogrel for a few months and aspirin for 6 months.
If any dental treatment involving bleeding, tooth extraction, or surgical intervention is needed within the first 6 months after the ASD closure procedure, the patient should receive antibiotic treatment, which should be prescribed by the performing cardiologist.
What are the advantages of non-surgical closure of ASD compared to the surgical method?
- The patient stays in the hospital for only 24 hours and can return to work after resting at home for one to two days.
- Unlike the surgical method, there is no need to open the chest or connect to a heart-lung machine.
- There is no surgical scar on the chest from an aesthetic standpoint.
- The risk of death due to the procedure is much lower compared to surgery.
What is the risk of non-surgical ASD closure?
Although rare, there are some risks involved. There might be puncture bleeding along the length of the vessel where the closure device is advanced, and there is a possibility of perforation or tearing of the heart walls. The closure device might also dislodge into the heart or vessel, necessitating surgical intervention and blood transfusion.
In rare cases, post-procedural infections might occur, requiring antibiotic treatment. Additionally, the patient may rarely experience a stroke during or after the procedure, leading to functional impairment. Heart rhythm disturbances may also develop during or after the procedure.
The device left in place might potentially damage the surrounding heart tissues, necessitating correction through surgery. In rare instances, clot formation on the closure device might lead to embolism. While highly uncommon, the non-surgical ASD closure procedure can lead to the patient’s death.
What is VSD (Ventricular Septal Defect)?
When there is a hole in the partition between the atria, this hole is referred to as an ASD (atrial septal defect), or if the shape and function of this hole differ, it is referred to as a PFO (patent foramen ovale). The ventricles are separated from each other by a wall of heart muscle.
When there is a hole in the wall or partition (ventricular septum) separating the left and right ventricles, this hole is called a VSD (ventricular septal defect). In the presence of a VSD, clean blood from the left ventricle flows into the right ventricle, increasing the volume of blood that the right heart needs to pump to reach the lungs.
Over time, this leads to an increase in pressure in the right ventricle and an excessive volume load in the left ventricle, increasing the workload of both ventricles. If too much blood is crossing from left to right, this condition can lead to heart failure and pulmonary hypertension (increased pressure in the pulmonary artery).
If this condition is not treated before reaching an irreversible stage, the patient will live with heart failure problems for life and typically die at an early age. Additionally, the presence of a VSD can lead to infective endocarditis, a laborious and potentially fatal heart valve inflammation.
VSDs located just below the aortic valve can cause aortic valve insufficiency, which needs to be corrected surgically.
How is VSD treated?
If the amount of blood flowing from left to right through the VSD is significant, the VSD should be closed; otherwise, irreparable damage may occur in the heart.
Surgical treatment: The chest cavity is opened with open-heart surgery, and the hole is repaired or patched using surgical methods.
Perkutanous treatment: Also known as non-surgical or umbrella method. It is a preferred method over surgery in suitable cases. In the non-surgical approach, a needle is inserted into the femoral vein and artery through the groin, and a vascular sheath is placed in both vessels.
A catheter and guide wire inserted through the femoral artery is advanced to the heart, passing through the hole (VSD). This allows access to the right heart, where the guide wire is snared within the heart or pulmonary artery, then pulled back and removed from the femoral vein (groin).
This creates a system with a guide wire entering from one sheath and exiting from the other. Through the guide wire inserted from the femoral vein, a VSD closure device delivery catheter is sent, passing through the VSD and into the left ventricle or even the aortic valve to reach the aorta.
VSD closure devices are connected disks, and the closure device, selected according to the VSD size, is advanced through the delivery catheter to the tip of the catheter.
In the left ventricle, the catheter tip is pulled out, and the first disk of the device is opened and pulled back to be placed inside the VSD, and the second disk of the device is also opened on the right ventricle side, closing the VSD.
Consequently, the first disk of the closure device closes the opening facing the left ventricle, and the second disk closes the opening facing the right ventricle. The delivery catheter is withdrawn, and the procedure is completed.
The endocardium, which covers the inside of the heart, eventually covers the closure device, completely coating it with endocardial cells within an average of 3-6 months. The closure device remains in place.
Some individuals may have allergies to the materials used in these closure devices, and this should be investigated before the procedure. The non-surgical VSD closure procedure typically takes about 1 hour, and the patient may be sedated for about half an hour during the procedure.
This is not general anesthesia but is referred to as deep sedation or deep sleep, and the patient is awakened immediately after the procedure. In some cases, the procedure can be performed while the patient is awake.
After the procedure, the patient remains in bed for at least 6 hours and stays overnight in the hospital, then is discharged in the morning. To prevent clot formation on the closure device, it is recommended to use clopidogrel for several months and aspirin for 6 months.
Within the first 6 months after the VSD closure procedure, if any dental treatment involving bleeding, tooth extraction, or any surgical intervention is necessary, the patient should receive antibiotic treatment, which should be done in consultation with the performing cardiologist.
What are the advantages of percutaneous treatment?
The hospital stay is much shorter compared to surgery (24 hours). In the surgical method, opening the chest results in a large surgical scar on the chest. Percutaneous closure can also be preferred for aesthetic reasons.
What is the risk of non-surgical VSD closure?
Although rare, there are some risks involved. There may be puncture bleeding in the vessel where the closure device is advanced, as well as perforation and tearing of the heart walls. The closure device may fall into the heart or the vessel, necessitating surgical intervention and blood transfusion.
Rarely, an infection may occur after the procedure, requiring antibiotic treatment. Additionally, the patient may rarely experience a stroke and functional loss.
During and after the procedure, there may be the development of irregular heart rhythms, and the heart rate may slow down significantly, necessitating the installation of a pacemaker.
The surrounding heart tissues may be damaged after the device is released, requiring correction through surgery. Blood clots may form on the closure device, leading to embolism. Although very rare, the non-surgical VSD closure procedure can lead to the patient’s death.
Post-Procedure Follow-Up
After the procedure, the patient stays in the coronary intensive care unit for one night and can be discharged the following day. Within a few days, they can return to their normal life and work.
To prevent clot formation on the device, it is recommended to use clopidogrel for several months and aspirin for 6 months.
Within the first 6 months after the VSD closure procedure, if there is a need for dental treatment, tooth extraction, or any surgical intervention, the patient should receive antibiotic treatment, which should be consulted with the cardiologist performing the procedure.